Explore the crucial world of EMR Integration in healthcare. This article provides insights into the essential role of Electronic Medical Records (EMR) and its integration, shedding light on market trends and its impact on healthcare technology.
What You Will Learn:
- Uncover the importance of EMR in the rapidly growing healthcare sector.
- Understand the key functions of EMR, such as charting, patient portals, e-prescribing, and more.
- Discover market trends, with the global EMR market set to double its revenue by 2028.
- Explore the need for EMR integration, including types, benefits, and core standards.
- Learn about crucial types of EMR integration systems, their benefits, and challenges.
Immerse yourself in the world of EMR Integration, gaining valuable insights into its significance and practical applications in healthcare technology.
- The importance of EMR integration in Healthcare
- Types of EMR integration systems in Healthcare
- 1. Laboratory Information System (LIS)
- 2. Clinical Trial Management System (CTMS)
- 3. Medical Billing
- 4. Medical Device Integration (MDI)
- 5. Telehealth
- 1. Cloud Healthcare EMR Integration
- 2. Mac EMR Healthcare Integration
- 3. ONC-Certified EMR Healthcare Integration
- 4. Behavioral/Mental Health EMR Healthcare Integration
- Benefits of Using EMR Integrations for Healthcare Development
- Real-time Data Access and Analytics
- Reduce Data Entry
- Increased Practice Productivity and Improved Patient Care
- Enable Innovation
- Patient Satisfaction
- Enhanced Communication
- Government Incentives
- Core Standards of EMR Integration for Healthcare Technical Products
- Final Thoughts
- Consider Inoxoft as a Reliable Partner for Developing Products in Healthcare Industry
The healthcare industry has been growing at the speed of light. No wonder there was and is such a great demand for medical solutions. Also, diseases don’t simply disappear. They might be chronic and based on the global ecological changes. Or, on the contrary – human-produced and the ones that mutated. For example, take into account COVID-19 alone. Or the new-spreading viral monkeypox. Humanity needs healthcare to be quick and operative more than ever today. So, there are numerous market offerings. One of such offerings is digital health technology or the traditional EMR/EHR.
In fact, what is an Electronic Medical Record (EMR)?
A digital health record of a patient’s health information that has been collected systematically and stored within a healthcare system.
The key functions of any EMR system include
- Charting
- Patient Portals
- E-Prescribing
- Order Entry
- Decision Support
In 2020, the market size of the EMR market worldwide was valued at $29 billion. With the recent industry innovations and constant development of medical apps, the market revenue is to double by 2028. So, the EMR market is to expand at a CAGR of 6.9% to $42,818 million.
Furthermore, EMR in the healthcare setting has to be integrated into a medical system first. Then, you will be able to use it correctly. Thus, the article will speak about:
- healthcare EMR integration
- types of EMR integration
- benefits of EMR integration for healthcare
- core standards of EMR integration
If you still don’t know all the details about EMR integrations for healthcare – read this article!
The importance of EMR integration in Healthcare
An EMR integration helps to connect an EMR platform with other healthcare systems. It allows a better flow of medical data and enhances interoperability between these digital health tools.
The most crucial usage of EMR is in patient record management. Medical circles have always produced lots of patient data and stored and accessed it when necessary. If these records were manually written, they could have easily been lost, mixed up, etc. Human error is one of the biggest threats to modern healthcare provision.
So,
EMR is designed to store patient treatment records, charts, test results, etc. Thanks to it, you can easily access, manage and retrieve patient data.
Continuous care is a highly-valued prerogative. And, to make it possible, any medical institution should gather and form a comprehensive picture of patient history. It should be accessible, readable, and logically structured.
– Would EMR improve patient care? – Surely!
– Would it reduce errors during manual paperwork? – Yes, definitely!
– Would EMR lower the costs? – Partially but yes!
– Would it enhance practice operations? – By all means!
As for the development of digital healthcare, such an integrated practice is the safety boat for many patients. Their records will be in one place, safe and securely stored, with physicians’ access 24/7 and their own. That’s why EMR is a great tool for industry advancement. With the practice management of EMR, the e-health sector can manage patient care flexibly.
Types of EMR integration systems in Healthcare
There are at least 5 systems a single EMR can integrate with. These are
1. Laboratory Information System (LIS)
Back in the day, to pass blood tests or any other type of testing was equal to passing circles and circles of medical cabinets. First, you had to go to your family doctor. Second, a physician had to prescribe you those tests on a blank of paper (fill out an order). And, third, you took this blank and went to the right laboratories, stood in queues, etc. All in all, to collect results you had to go to the laboratories and ask for them to be printed out. But mostly, they were handwritten. Maybe, not all the countries had such processes, but the third-world ones still have. Partially, in governmental medical institutions and clinics.
Most private medical facilities changed their testing procedures with the help of LIS. Now, you take the doctor’s order, go straight into the laboratory, pass everything that the system uploads from your doctor’s check-up and receive results in the private account. Your doctor can see them as well. Consequently, it is the future. And, it is super convenient.
2. Clinical Trial Management System (CTMS)
CTMS refers to clinical trials and research. It exists as a measure of patient safety. Doctors need to have access to information about the clinical trial enrollment of their patients. This is crucial as the patient’s medical history is the primary source of information. It can reveal lots of factors and save doctors from erroneous decisions. CTMS integration has lots of advantages.
3. Medical Billing
EMR revolves around patient care, while the system of medical billing manages your revenue cycle. But, integrating with billing software should be a priority as it will increase reimbursement.
4. Medical Device Integration (MDI)
It depends on the size of your practice and your need to understand whether you should implement this MDI – EMR integration for healthcare. But, ICU and OR departments in clinics use many devices and EMR integration tools like monitors, smart beds, anesthesia carts, finger cuffs, and ventilators. These show the current situation with vital signs (blood pressure, heart rate, and oxygen saturation).
The main thing is that these devices produce lots of data, which is critical to both patients and their care providers. And MDI is just the tool, which automates the data transfer of all the devices to the EMR.
5. Telehealth
Telehealth applications became popular with the outbreak of COVID-19. However, they stayed popular afterward. Mainly, because they are virtual. And, integrated electronic health records with such a virtual solution can be a potential benefit. This kind of integration provides practitioners with an end-to-end bidirectional interface. It allows the passing of patients’ data forward and backward between systems.
But EMR integrations for the Healthcare industry with different medical systems also have several other options:
1. Cloud Healthcare EMR Integration
Via this integration option, you can access data online. Because a cloud solution gathers and stores all the patient information “in the cloud” of an EMR. And, it is quite affordable. It is also called a SaaS or web-based cloud software that hosts data.
2. Mac EMR Healthcare Integration
This type of integration requires an Apple device. It is specifically designed and adjusted to the Mac OS. Also, consider cloud/web software that runs on Apple devices that have Internet access.
3. ONC-Certified EMR Healthcare Integration
The Office of the National Coordinator for Health Information Technology has specific requirements for software development and integration. These requirements include rules according to proper management and storage of sensitive patient data. So, there are criteria the EMR has to follow. These criteria include patient portal access, a place to create care plans, quality reporting methods, etc.
4. Behavioral/Mental Health EMR Healthcare Integration
EMR integration solutions for mental health and behavioral health purposes have various features. Each of the needs is specific to the clinics or the therapist. Accessing lab results, notes, patient history, and a chronological treatment plan can be an easy task with the help of an EMR integration.
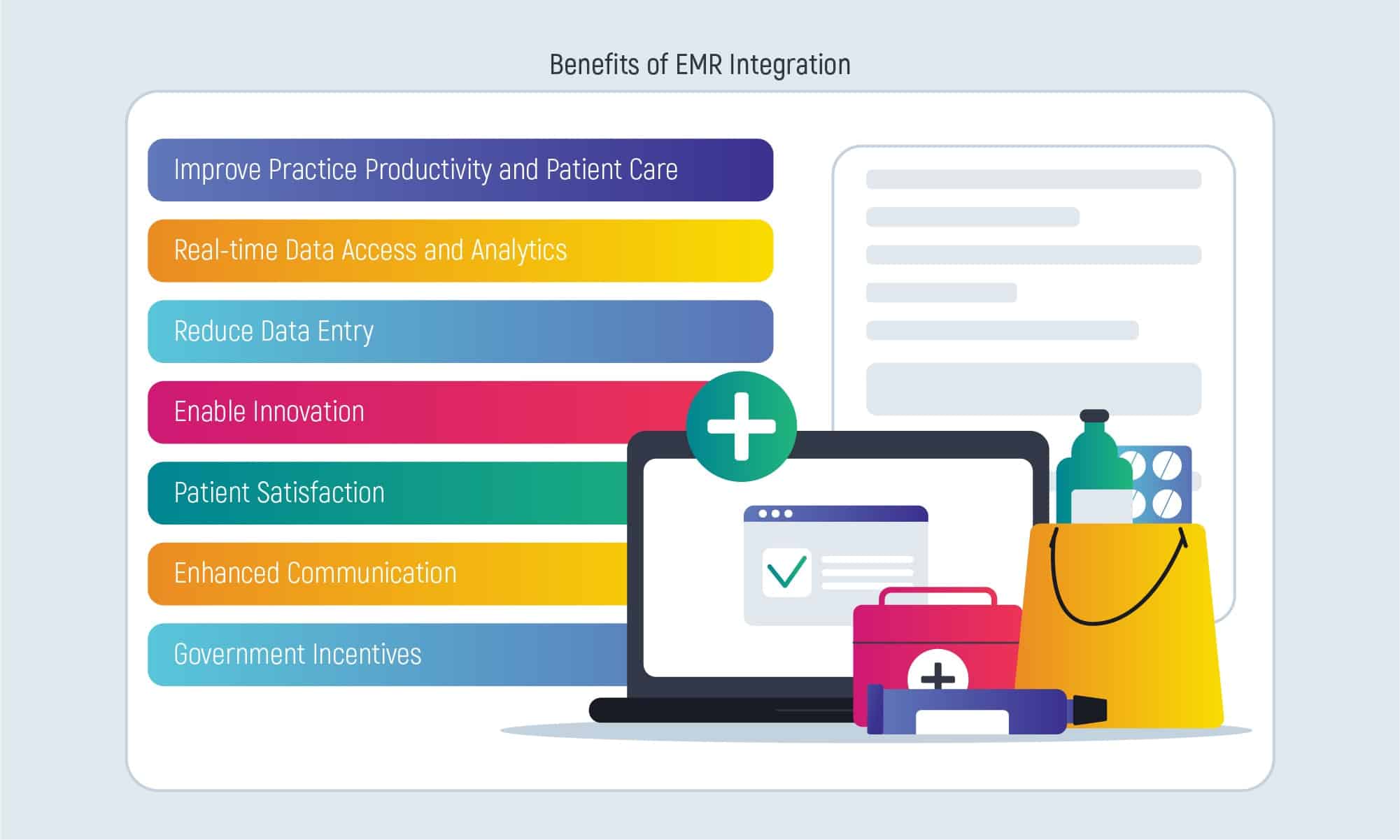
Benefits of Using EMR Integrations for Healthcare Development
Real-time Data Access and Analytics
With EMR integration in healthcare products, both the patient and the doctor have round-the-clock access to a patient record. EMR gathers data from all medical systems (or devices). It gradually improves data collection during treatment and creates a centralized repository of data that is extra accessible.
Reduce Data Entry
Can potentially reduce errors and unnecessary time consumption that happens during data transcription. Clinical data is being transcripted in any medical system once. Afterward, this transcription is uploaded to all the other clinical systems.
Increased Practice Productivity and Improved Patient Care
EMR saves a lot of time on both sides. All of it is due to easier access, reduced data entry, and the possibility to provide better patient care simultaneously. If doctors can visualize and read patient history to the slightest details – patient outcome improves significantly. To coordinate care in a better way, there’s a connected ecosystem of software and devices to do it.
Enable Innovation
Central repository created by the EMR and the data gateway with the uninterrupted flow of medical data belonging to IoT or IoMT (Internet of Medical Things). Both IoT and IoMT have a vast field to conquer and presuppose innovations coming one by one.
Patient Satisfaction
EMR integration systems in healthcare allow patients to interact with scheduling, pay online, set up different reminders and give feedback, etc. The ability to use such an advanced method of setting up doctor appointments, paying for the services via the Liqpay system (Apple Pay, Google Pay, etc.), working with your calendar to fit in the appointment, and giving feedback for the services allows patients to feel supported and taken care of right from the start. This is an evident plus to patient satisfaction.
Enhanced Communication
Among the advantages of EMR integration for healthcare there are several benefits:
- patient-doctor communication
- doctor-medical practices communication
- doctor-pharmacies communication
- doctor-laboratories communication
This allows to improve connectivity with the other clinical departments and set up a good working environment.
Government Incentives
It depends on your location, but most governmental programs include incentive programs offered to clinicians as a benefit of implementing EMRs. Incentives tend to encourage interoperability to improve patient outcomes.
Core Standards of EMR Integration for Healthcare Technical Products
Like there are development standards for any other products, there are standards and compliance for EMR integration for healthcare tech products. These standards include:
- Core functional requirements
- Core technical requirements
Of course, there are other standards to include. Still, they will result in your primary need for EMR integration for the healthcare tech industry. To ensure, you know what you are doing, try answering the following questions:
- What are the goals of integrating an EMR?
- Who will use the EMR system?
- How many users will be involved?
- Which solutions the EMR system will integrate with?
- Should it be web or mobile or both – accessible?
- What do you expect of the integration performance?
Final Thoughts
Insights:
-
Evolution of Healthcare Technology: The rapid growth of the healthcare industry is driven by increasing demand for medical solutions, fueled by factors such as chronic illnesses and emerging diseases like COVID-19 and monkeypox. This necessitates the adoption of digital health technologies like Electronic Medical Records (EMRs) to meet the evolving needs of patients and healthcare providers.
-
Understanding EMRs: EMRs serve as comprehensive digital repositories of patient health information, offering functionalities such as charting, patient portals, e-prescribing, order entry, and decision support. The global EMR market witnessed substantial growth, reaching $29 billion in 2020, with projections to double by 2028, highlighting the industry’s trajectory towards digitalization.
-
Importance of EMR Integration: Integrating EMRs with other healthcare systems enhances interoperability and facilitates seamless data exchange, leading to improved patient care and operational efficiency. EMR integration is particularly crucial for patient record management, mitigating the risks associated with manual record-keeping and ensuring accessibility, accuracy, and security of patient data.
-
Types of EMR Integration Systems: EMRs can integrate with various healthcare systems, including Laboratory Information Systems (LIS), Clinical Trial Management Systems (CTMS), Medical Billing systems, Medical Device Integration (MDI), and Telehealth applications. Each integration type offers unique benefits, ranging from streamlining testing procedures to facilitating virtual consultations and remote monitoring.
-
Benefits of EMR Integrations: EMR integrations yield numerous benefits, including real-time data access and analytics, reduced data entry errors, increased practice productivity, improved patient care outcomes, enablement of innovation through IoT integration, enhanced patient satisfaction, improved communication among healthcare stakeholders, and eligibility for government incentive programs.
-
Core Standards for EMR Integration: Adhering to core functional and technical requirements is essential for successful EMR integration. Key considerations include defining integration goals, identifying end-users, determining the scale of integration, selecting compatible solutions, deciding on accessibility (web or mobile), and establishing performance expectations.
-
Enhancing Patient Care through Technology: EMR integration serves as a cornerstone for modern healthcare delivery, enabling healthcare providers to deliver patient-centered care, streamline workflows, and leverage data-driven insights for informed decision-making. By embracing technology and adhering to integration best practices, healthcare organizations can enhance efficiency, effectiveness, and patient satisfaction across the care continuum.
To conclude, the importance of EMR integrations for healthcare is quite obvious. Joining an EMR solution with other potentially beneficial systems in the medical setting allows the enhancement of all healthcare processes. Patients are satisfied with the fast and accurate health provision. Doctors have full access to patient data.
What’s more, the place for errors is extremely decreased. And, so are the costs for erroneous decisions. The workflow of a physician can become lighter and with a better focus on patients than data transitions from one department to the other. Patients can be sure their data won’t be lost in the process.
We can tell a lot more about EMR/EHR software. Here, you can find the pros and cons of electronic medical records.
Consider Inoxoft as a Reliable Partner for Developing Products in Healthcare Industry
Inoxoft is a healthcare development services company with 7+ years of experience. Our experts monitor the mhealth development services market and have a solid knowledge of the latest trends. EHRs/EMRs, Patient and Doctor communication apps, Wellness apps, Web responsive hospital-based apps, and chatbots are the main requests from our clients.
Inoxoft’s young team is happy to implement a healthcare app according to your requirements. We care both about your business growth and human well-being. Contact us and we will build a top-market solution together!
Frequently Asked Questions
What is the use of EMR integrations for healthcare?
The most crucial usage of EMR is in patient record management. Medical circles have always produced lots of patient data and it had to be stored and accessed when there was a need.
What are the EMR integration solutions for healthcare?
- Laboratory Information System (LIS)
- Clinical Trial Management System (CTMS)
- Medical Billing
- Medical Device Integration (MDI)
- Telehealth
- Cloud Healthcare EMR Integration
- Mac EMR Healthcare Integration
- ONC-Certified EMR Healthcare Integration
- Behavioral/Mental Health EMR Healthcare Integration
What is the healthcare EMR integration?
An EMR integration helps to connect an EMR platform with other healthcare systems. This allows a better flow of medical data and enhances interoperability between these digital health tools.