In this rapidly evolving digital era, the concept of a Virtual Health Assistant has gained significant momentum. A Virtual Health Assistant is an application or system that utilizes artificial intelligence (AI) and machine learning technologies to provide personalized healthcare services to individuals. This article will guide you through the process of building a Virtual Health Assistant, covering various aspects such as understanding its concept, selecting the right technologies, ensuring compliance with health regulations, testing and launching, and maintaining and improving the assistant post-launch.
- Understanding the Concept of a Virtual Health Assistant
- The role and importance of Virtual Health Assistants
- Key features of an effective Virtual Health Assistant
- Steps to Building Your Medical AI Assistant
- Selecting the Right Technologies for Your Virtual Health Assistant
- Overview of programming languages and platforms
- Choosing the right AI and machine learning tools
- Ensuring Compliance with Health Regulations
- Understanding HIPAA and other health data regulations
- Implementing security measures for patient data
- Testing and Launching Your Virtual Health Assistant
- Strategies for a successful launch
- Maintaining and Improving Your Virtual Health Assistant Post-Launch
- Gathering user feedback for continuous improvement
- Keeping up with technological advances and health trends
Understanding the Concept of a Virtual Health Assistant
Virtual Health Assistants have emerged as a transformative solution in the healthcare industry. These intelligent assistants enable individuals to access personalized healthcare services conveniently and efficiently. By utilizing AI and machine learning technologies, Virtual Health Assistants can assist users in various tasks, such as providing medical advice, scheduling appointments, monitoring health conditions, and offering lifestyle recommendations.
Virtual Health Assistants have revolutionized the way individuals interact with healthcare services. Gone are the days of long waits at the doctor’s office or struggling to find reliable health information online. With the help of AI Medical Assistant, individuals can now have instant access to a wealth of healthcare knowledge and resources.
The role and importance of Virtual Health Assistants
Virtual Health Assistants play a crucial role in enhancing the overall healthcare experience for individuals. They act as virtual companions, providing guidance, support, and relevant information to users whenever needed. Whether it’s a simple question about a medication or a more complex concern about a medical condition, Virtual Health Assistants are there to assist and empower individuals in making informed healthcare decisions.
One of the key importance of Virtual Health Assistants lies in their ability to improve healthcare accessibility. In many parts of the world, access to quality healthcare services is limited, especially in remote areas. Virtual Health Assistants bridge this gap by providing individuals with access to healthcare professionals and resources, regardless of their geographical location.
Additionally, Virtual Health Assistants have the potential to reduce healthcare costs. By offering personalized guidance and recommendations, individuals can better manage their health and prevent unnecessary visits to healthcare facilities. This not only saves money but also reduces the burden on healthcare systems, allowing them to allocate resources more efficiently.
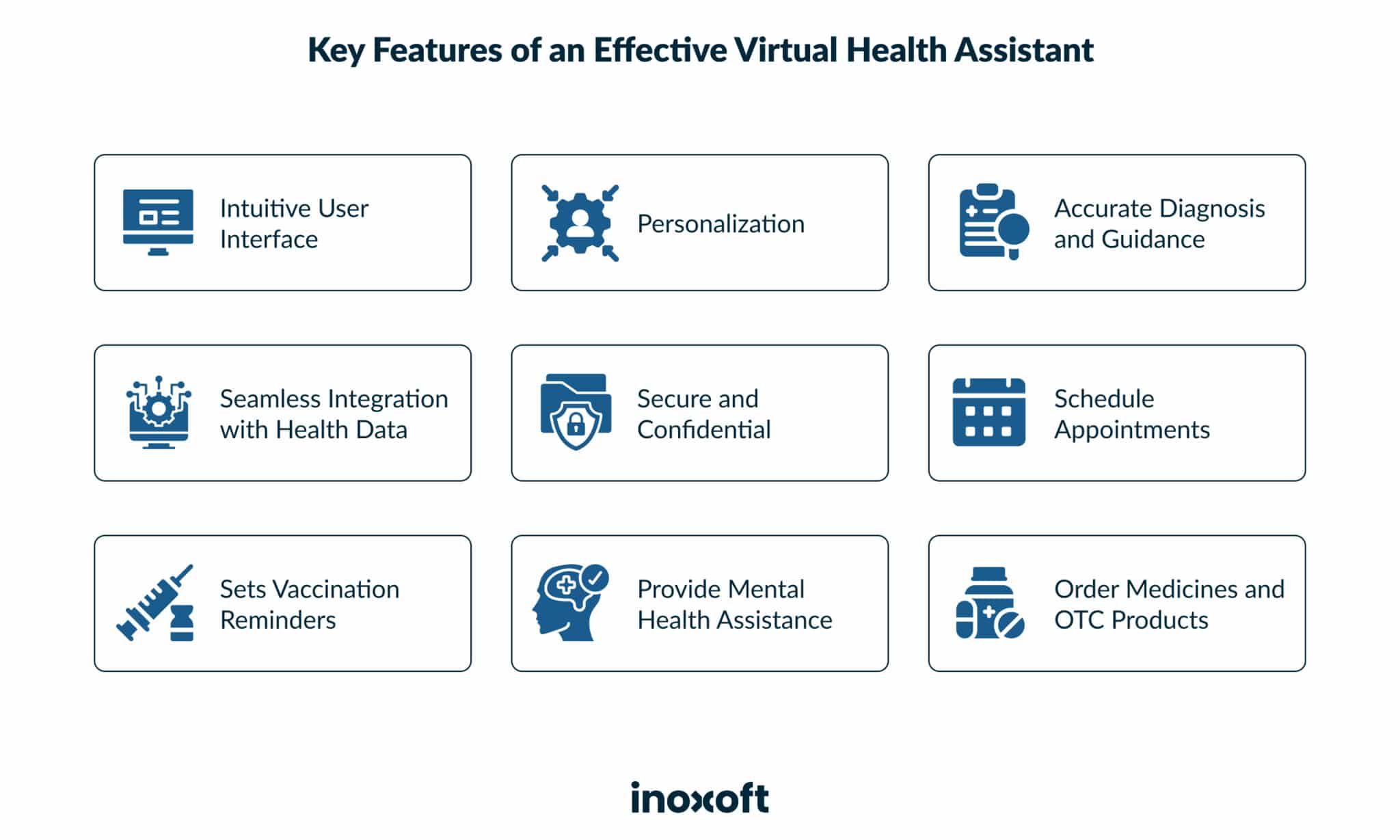
Key features of an effective Virtual Health Assistant
An effective Virtual Health Assistant should possess certain key features to ensure its usefulness and user-friendliness. These features include:
- Intuitive user interface
A well-designed interface that is easy to navigate and understand. A clutter-free and visually appealing interface can enhance the user experience and make interacting with the Virtual Health Assistant a breeze.
- Personalization
Tailoring recommendations and insights based on individual health data and preferences. Every individual is unique, and their healthcare needs may vary. A Virtual Health Assistant that can adapt to the user’s specific requirements can provide a more personalized and effective healthcare experience.
- Accurate diagnosis and guidance
The ability to provide accurate diagnoses based on symptoms and offer appropriate guidance. Virtual Health Assistants equipped with advanced AI algorithms can analyze symptoms and provide users with reliable information, helping them make informed decisions about their health.
- Seamless integration with health data
Integration with electronic health records (EHRs) and other health-related data sources. By seamlessly integrating with existing health data systems, Virtual Health Assistants can provide a comprehensive view of an individual’s health, enabling healthcare professionals to make more informed decisions.
- Secure and confidential
Ensuring the privacy and security of user data in compliance with regulations such as HIPAA. Virtual Health Assistants handle sensitive health information, and it is crucial that they maintain the highest standards of data security and confidentiality to protect user privacy.
By incorporating these key features, AI Medical Assistants can deliver a seamless and personalized healthcare experience to individuals. The future of healthcare is undoubtedly intertwined with the advancements in AI and machine learning, and Virtual Health Assistants are at the forefront of this revolution.
Steps to Building Your Medical AI Assistant
Building a Virtual Health Assistant requires a structured approach. Inoxoft – software development company has extensive expertise in healthcare software development and can assist you in each step of the process. The following steps outline the journey to building a successful Virtual Health Assistant:
1. Identifying the needs of your target audience
The first step in building a Virtual Health Assistant is to understand the specific needs and requirements of your target audience. Conduct thorough market research and user surveys to gain insights into the challenges individuals face in accessing healthcare services and their expectations from a Virtual Health Assistant. During the market research phase, it is important to gather data from a diverse range of sources. This can include conducting interviews with healthcare professionals, analyzing existing healthcare apps and platforms, and studying industry reports and trends. By gathering a comprehensive understanding of your target audience’s needs, you can ensure that your Virtual Health Assistant is designed to address their specific pain points. Once you have gathered the necessary data, it is important to analyze and categorize the information. This will help you identify common themes and patterns, which can then be used to inform the design and development of your Virtual Health Assistant.
2. Designing the user interface
Once you have a clear understanding of your target audience’s needs, the next step is to design an intuitive and user-friendly interface. The user interface should be visually appealing, easy to navigate, and responsive across different devices and platforms. Collaborate with experienced UI/UX designers to create a seamless user experience. During the design phase, it is important to consider the unique requirements of a Virtual Health Assistant. This may include incorporating features such as appointment scheduling, medication reminders, and real-time communication with healthcare professionals. By working closely with UI/UX designers, you can ensure that the user interface is tailored to meet the specific needs of your target audience. Once the initial design concepts have been created, it is important to gather feedback from potential users. This can be done through usability testing and focus groups. By involving your target audience in the design process, you can gather valuable insights and make any necessary adjustments to improve the user experience.
3. Developing the backend and algorithms
The backbone of any Virtual Health Assistant lies in its backend infrastructure and algorithms. This entails developing robust systems to handle data storage, data processing, and integrating AI and machine learning algorithms. During the development phase, it is important to prioritize security and privacy. Healthcare data is highly sensitive, and it is crucial to implement measures to protect patient information. This can include encryption protocols, secure authentication methods, and regular security audits. In addition to the backend infrastructure, the development phase also involves integrating AI and machine learning algorithms. These algorithms can help improve the accuracy and efficiency of the Virtual Health Assistant. For example, machine learning algorithms can be used to analyze patient data and provide personalized recommendations for treatment plans. Throughout the development process, it is important to conduct regular testing and quality assurance checks. This will help identify and address any bugs or issues before the Virtual Health Assistant is launched to the public.
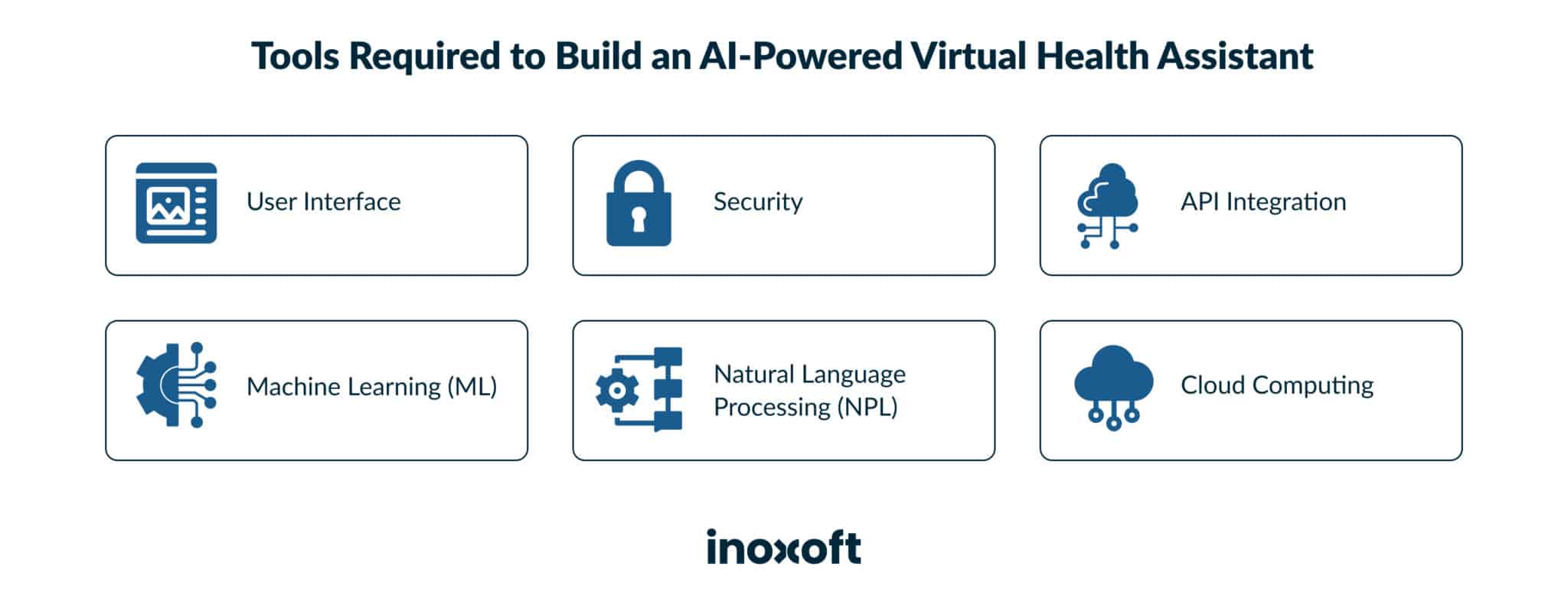
Selecting the Right Technologies for Your Virtual Health Assistant
The success of your Virtual Health Assistant depends on choosing the right technologies to support its functionalities. Inoxoft can consult you on the following:
Overview of programming languages and platforms
When it comes to developing Virtual Health Assistants, there are several programming languages and platforms to choose from. Each option has its own strengths and weaknesses, and the selection should be based on the specific requirements and scalability needs of your Virtual Health Assistant.
Python is a popular choice for developing Virtual Health Assistants due to its simplicity and versatility. It has a wide range of libraries and frameworks that can be used to implement various functionalities, such as data analysis, machine learning, and natural language processing.
Java is another widely used programming language for developing Virtual Health Assistants. It is known for its robustness and scalability, making it suitable for large-scale applications. Java also has a strong ecosystem of libraries and frameworks that can be leveraged to enhance the capabilities of your Virtual Health Assistant.
Ruby on Rails is a web development framework that can be used to build Virtual Health Assistants. It is known for its simplicity and convention-over-configuration approach, which can help speed up the development process. Ruby on Rails also has a strong community and a rich ecosystem of plugins and gems that can be utilized to add additional functionalities to your Virtual Health Assistant.
Choosing the right AI and machine learning tools
Medical assistant and AI technology are the driving force behind the intelligence of Virtual Health Assistants. Selecting the right AI and machine learning tools, libraries, and frameworks is crucial for developing accurate diagnosis algorithms, personalized recommendations, and natural language processing capabilities.
Several popular AI and machine learning tools can be used in the development of Virtual Health Assistants:
- TensorFlow is an open-source library developed by Google that provides a wide range of tools and resources for building machine learning models. It has a strong community and extensive documentation, making it a popular choice among developers.
- Another popular choice is PyTorch, an open-source machine learning library developed by Facebook. PyTorch is known for its dynamic computational graph, which allows for more flexibility in model development. It also has a rich ecosystem of libraries and frameworks that can be used to enhance the capabilities of your Virtual Health Assistant.
- Scikit-learn is a machine learning library for Python that provides a wide range of algorithms and tools for data analysis and modeling. It is known for its simplicity and ease of use, making it a good choice for developers who are new to machine learning.
By carefully selecting the right AI and machine learning tools, libraries, and frameworks, you can ensure that your Virtual Health Assistant is equipped with the necessary intelligence to provide accurate diagnoses, personalized recommendations, and seamless natural language processing capabilities.
Ensuring Compliance with Health Regulations
When developing a Virtual Health Assistant, it is vital to comply with health regulations and ensure the security and confidentiality of patient data. Inoxoft can help you navigate the complexities of compliance by:
Understanding HIPAA and other health data regulations
The Health Insurance Portability and Accountability Act (HIPAA) sets standards for protecting sensitive patient health information. It is essential to understand the requirements and guidelines of HIPAA and other relevant health data regulations to ensure the legal and ethical use of data.
Complying with HIPAA and other health data regulations involves more than just following a set of rules. It requires a deep understanding of the healthcare industry, the intricacies of patient data, and the potential risks associated with mishandling such information. Inoxoft has a team of experts who are well-versed in these regulations and can guide you through the process of compliance.
By understanding HIPAA and other health data regulations, you can ensure that your Virtual Health Assistant is designed and developed in a way that respects patient privacy and confidentiality. This includes implementing appropriate data access controls, encryption methods, and secure storage practices.
Implementing security measures for patient data
Data security is of utmost importance in healthcare. Implementing robust security measures, such as encryption, access controls, and regular security audits, will help safeguard patient data and maintain trust in your Virtual Health Assistant.
When it comes to patient data, there is no room for compromise. Inoxoft understands the critical nature of protecting patient information and can help you implement the necessary security measures to ensure the confidentiality and integrity of data.
- Encryption is a fundamental aspect of data security. By encrypting patient data, you can ensure that even if it falls into the wrong hands, it remains unreadable and unusable. Inoxoft can assist you in implementing encryption protocols that meet industry standards and comply with health regulations.
- In addition to encryption, access controls play a crucial role in maintaining data security. By implementing access controls, you can restrict access to patient data to only authorized individuals. Inoxoft can help you design and implement access control mechanisms that align with your specific needs and comply with health regulations.
- Regular security audits are essential to identify and address any vulnerabilities in your Virtual Health Assistant’s security infrastructure. Inoxoft can conduct comprehensive security audits to ensure that your system is robust and resilient against potential threats.
By partnering with Inoxoft, you can rest assured that your Virtual Health Assistant will comply with health regulations and prioritize the security and confidentiality of patient data.
Testing and Launching Your Virtual Health Assistant
Before launching your Virtual Health Assistant, rigorous testing is essential to ensure its functionality and accuracy. Collaborate with QA specialists to perform comprehensive testing, including user acceptance testing, performance testing, and security testing. Once the testing phase is complete, you can proceed with launching your Virtual Health Assistant.
Testing a Virtual Health Assistant involves a meticulous process to ensure that it meets the highest standards of quality. QA specialists work closely with developers to identify and fix any potential issues or bugs that may arise during the testing phase.
- Functional testing is conducted to verify that all the features and functionalities of the Virtual Health Assistant are working as intended. This includes testing the accuracy of medical information provided by the assistant, as well as its ability to handle user queries and provide appropriate responses.
- Usability testing is also performed to evaluate the user-friendliness of the interface and ensure that users can easily navigate through the application.
- Compatibility testing is crucial to ensure that the Virtual Health Assistant works seamlessly across different devices and platforms. This includes testing the application on various operating systems, browsers, and screen sizes to ensure that it provides a consistent user experience regardless of the device being used.
- Performance testing is another important aspect of the testing process. It involves assessing the Virtual Health Assistant’s performance under different scenarios, such as high user loads or simultaneous user interactions. This helps identify any performance bottlenecks and ensures that the application can handle the expected user traffic without any degradation in performance.
By conducting rigorous testing, you can identify and address any potential issues or bugs in your Virtual Health Assistant before launching it to the public. This helps ensure that users have a positive experience and can rely on the assistant for accurate and reliable health information.
Strategies for a successful launch
A successful launch requires a well-planned marketing and communication strategy. Generate awareness about your Virtual Health Assistant through various channels, such as social media, healthcare forums, and partnerships with healthcare providers. By leveraging social media platforms, you can reach a wide audience and engage with potential users. Healthcare forums provide an opportunity to connect with healthcare professionals and enthusiasts who may be interested in your Virtual Health Assistant. Collaborating with healthcare providers allows you to tap into their existing patient base and gain credibility in the industry.
In addition to marketing efforts, continuously gathering feedback from users is crucial for the success of your Virtual Health Assistant. Actively listen to user feedback and iterate on your assistant based on their needs and preferences. This iterative approach ensures that your Virtual Health Assistant evolves and improves over time, meeting the changing needs of users.
Furthermore, establishing a strong support system is essential to address any user concerns or issues. Provide clear channels of communication for users to reach out for assistance or report any problems they encounter. Promptly addressing user concerns helps build trust and confidence in your Virtual Health Assistant.
Launching a Virtual Health Assistant is an exciting endeavor, but it requires careful planning and execution. By conducting testing and implementing effective marketing and communication strategies, you can ensure a successful launch and provide users with a valuable and reliable tool for their healthcare needs.
Maintaining and Improving Your Virtual Health Assistant Post-Launch
The journey of building a Virtual Health Assistant does not end with its launch. Continuous maintenance, improvement, and adaptation are essential to ensure the long-term success of your assistant.
Gathering user feedback for continuous improvement
Actively seek user feedback on your Virtual Health Assistant’s performance, user experience, and features. Analyze the feedback and iterate on your Virtual Health Assistant regularly to address user concerns, improve its functionalities, and incorporate new features.
Keeping up with technological advances and health trends
The healthcare industry is constantly evolving with new technologies and health trends. Stay informed about the latest advancements in AI, machine learning, and digital health to keep your Virtual Health Assistant up-to-date and provide users with the most innovative solutions.
Frequently Asked Questions
What is a Virtual Health Assistant?
A Virtual Health Assistant is an AI-powered application or system that provides personalized healthcare services, such as medical advice, appointment scheduling, and lifestyle recommendations, to individuals.
How can a Virtual Health Assistant benefit healthcare providers?
Virtual Health Assistants can enhance healthcare providers' efficiency by reducing the burden of routine tasks, enabling remote patient monitoring, and facilitating easier access to patient health data.
Is it safe to store and share patient data with a Virtual Health Assistant?
Yes, it is safe to store and share patient data with a Virtual Health Assistant when appropriate security measures, such as encryption and access controls, are implemented. Compliance with health data regulations, such as HIPAA, is crucial to ensure data privacy and security.